Acetaminophen: Difference between revisions
imported>Robert Badgett (→Fever) |
mNo edit summary |
||
| (14 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{subpages}} | {{subpages}} | ||
{{TOC|left}} | |||
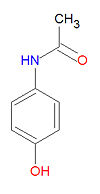
{{Image|Acetaminophen structure.jpg|right|100px|Acetaminophen (paracetamol)}} | |||
'''Acetaminophen''', also widely called '''acetaminofen''', '''paracetamol''' or '''paracetanol''', is an [[analgesic]] and [[antipyretic]] drug widely used for the treatment of [[headache]]s, [[fever]] and other minor aches and [[pain]]s. Many [[Common cold|cold]] and [[influenza|flu]] medications and some prescription analgesics contain acetaminophen. It has no mood altering effects and is not addictive although it can be combined with | '''Acetaminophen''', also widely called '''acetaminofen''', '''paracetamol''' or '''paracetanol''', is an [[analgesic]] and [[antipyretic]] drug widely used for the treatment of [[headache]]s, [[fever]] and other minor aches and [[pain]]s. Many [[Common cold|cold]] and [[influenza|flu]] medications and some prescription analgesics contain acetaminophen. Although it is sold under hundreds of names, it is popularly known as '''Tylenol'''®. | ||
The drug has long been considered especially safe, and replaced [[aspirin]] for many over-the-counter uses. It does not interfere with clotting mechanisms and increase bleeding tendency, and does not produce [[Reye's Syndrome]] in children. Nevertheless, suspicions arose that it could cause liver failure in heavy users of alcohol, but more data suggests there is a more general risk to the liver. In July 2009, an advisory committee to the [[Food and Drug Administration]] recommended that the maximum dose be reduced to 650 milligrams, from 1000 milligrams in current "extra strength" preparations. <ref name=FDAcomm>{{citation | |||
| title = FDA May Restrict Acetaminophen: Advisers Tell the Agency to Lower Over-the-Counter Dose of Popular Pain Drug | |||
| author = Kathryn Foxhall | |||
| journal = WebMD Health News | |||
| url = http://www.webmd.com/pain-management/news/20090701/fda-may-restrict-acetaminophen}}</ref> | |||
It has no mood altering effects and is not addictive although it can be combined with [[opioid analgesic]]s which have these effects such as oxycodone or hydrocodone with the brand names of Percocet and Vicodin respectively. These combinations do offer some synergistic pain control, but that is not the primary purpose. Indeed, some prescribers may recommend that before increasing opioid dose, a second 300-375mg acetaminophen be taken with the combined tablet. | |||
When the other drugs contain [[opioid analgesic]]s, the primary purpose is to keep the oral dose from being diverted to recreational injection. The combination also has some therapeutic sense, because acetaminophen and opioids affect different mechanisms of pain. Unfortunately, there have been cases where raising the combined-tablet dose, usually to provide more opioid and often under medical orders, inadvertently produced acetaminophen toxicity. The FDA Advisory committee recommended, with a 20 to 17 vote, that prescription products that combine acetaminophen with other medications should be eliminated.<ref name=FDAcomm /> This does not affect over-the-counter cold products that combine acetaminophen with such other agents as decongestants and cough supressants, but addresses the situation when the patient might try to increase pain relief with what would be a safe additional opioid dosage, but overdose with acetaminophen. There is little reason to take higher dose of a cold medication. | |||
==Pharmacology== | |||
==Mechanism of action== | |||
Acetaminophen inhibits [[cyclooxygenase]]-1 (COX-1) and [[cyclooxygenase]]-2 (COX-2) indirectly through a hypothesized yet unknown enzyme called COX-3, in the [[central nervous system]] and endothelial cells and thus suppresses the synthesis of [[prostaglandin]] and heightens the pain threshold. However, it does not inhibit COX enzymes in the peripheral tissues, and thus has no peripheral anti-inflammatory effects. | |||
===Metabolism=== | |||
[[Glucuronosyltransferase]] is part of the phase II drug metabolism of acetaminophen.<ref name="pmid10427468">{{cite journal| author=de Wildt SN, Kearns GL, Leeder JS, van den Anker JN| title=Glucuronidation in humans. Pharmacogenetic and developmental aspects. | journal=Clin Pharmacokinet |year= 1999 | volume= 36 | issue= 6 | pages= 439-52 | pmid=10427468 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=10427468 }} </ref> | |||
==Effectiveness== | ==Effectiveness== | ||
===Analgesia=== | ===Analgesia=== | ||
Acetaminophen one gram orally four times a day had similar efficacy to [[ibuprofen]] in reducing pain in [[randomized controlled trial]] of patients with mild to moderate [[osteoarthritis]] or the hip or knee.<ref name="pmid2052056">{{cite journal |author=Bradley JD, Brandt KD, Katz BP, Kalasinski LA, Ryan SI |title=Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee |journal=N. Engl. J. Med. |volume=325 |issue=2 |pages=87–91 |year=1991 |pmid=2052056 |doi=}}</ref> | Acetaminophen one gram orally four times a day had similar efficacy to [[ibuprofen]] in reducing pain in [[randomized controlled trial]] of patients with mild to moderate [[osteoarthritis]] or the hip or knee.<ref name="pmid2052056">{{cite journal |author=Bradley JD, Brandt KD, Katz BP, Kalasinski LA, Ryan SI |title=Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee |journal=N. Engl. J. Med. |volume=325 |issue=2 |pages=87–91 |year=1991 |pmid=2052056 |doi=}}</ref> | ||
"Diclofenac and paracetamol had the same effect on pain reduction of ankle sprains but more acute ankle edema was present in patients who were treated with diclofenac than in patients who were treated with paracetamol"according to a [[randomized controlled trial]]. <ref name="pmid21733417">{{cite journal| author=Lyrtzis C, Natsis K, Papadopoulos C, Noussios G, Papathanasiou E| title=Efficacy of paracetamol versus diclofenac for Grade II ankle sprains. | journal=Foot Ankle Int | year= 2011 | volume= 32 | issue= 6 | pages= 571-5 | pmid=21733417 | doi=10.3113/FAI.2011.0571 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21733417 }} </ref> | |||
Intravenous acetaminophen one gram was as effective as [[morphine]] 0.1 mg/kg for [[renal colic]].<ref name="pmid19647342">{{cite journal| author=Bektas F, Eken C, Karadeniz O, Goksu E, Cubuk M, Cete Y| title=Intravenous paracetamol or morphine for the treatment of renal colic: a randomized, placebo-controlled trial. | journal=Ann Emerg Med | year= 2009 | volume= 54 | issue= 4 | pages= 568-74 | pmid=19647342 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&email=badgett@uthscdsa.edu&retmode=ref&cmd=prlinks&id=19647342 | doi=10.1016/j.annemergmed.2009.06.501 }}</ref> | |||
====Combination therapy==== | |||
According to a [[systematic review]] sponsored by industry, combining acetaminophen with [[Non-steroidal anti-inflammatory agent]]s may help treatment of posteroperative pain.<ref name="pmid20142348">{{cite journal| author=Ong CK, Seymour RA, Lirk P, Merry AF| title=Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. | journal=Anesth Analg | year= 2010 | volume= 110 | issue= 4 | pages= 1170-9 | pmid=20142348 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20142348 | doi=10.1213/ANE.0b013e3181cf9281 }} </ref> | |||
For [[lumbalgia]], acetaminophen one gram orally four times a day combined with [[diclofenac]], a [[non-steroidal anti-inflammatory agent]], was not better than acetaminophen alone in a [[randomized controlled trial]].<ref name="pmid17993364">{{cite journal |author=Hancock MJ, Maher CG, Latimer J, ''et al'' |title=Assessment of diclofenac or spinal manipulative therapy, or both, in addition to recommended first-line treatment for acute low back pain: a randomised controlled trial |journal=Lancet |volume=370 |issue=9599 |pages=1638–43 |year=2007 |pmid=17993364 |doi=10.1016/S0140-6736(07)61686-9}}</ref> | |||
Acetaminophen has been combined with [[ibuprofen]] with uncertain results.<ref name="pmid21804100">{{cite journal| author=Doherty M, Hawkey C, Goulder M, Gibb I, Hill N, Aspley S et al.| title=A randomised controlled trial of ibuprofen, paracetamol or a combination tablet of ibuprofen/paracetamol in community-derived people with knee pain. | journal=Ann Rheum Dis | year= 2011 | volume= 70 | issue= 9 | pages= 1534-41 | pmid=21804100 | doi=10.1136/ard.2011.154047 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21804100 }} </ref> | |||
===Fever=== | ===Fever=== | ||
For reducing [[fever]], acetaminophen combined with [[ibuprofen]] may be better than either drug alone according to a [[randomized controlled trial]].<ref name="pmid18765450">{{cite journal |author=Hay AD, Costelloe C, Redmond NM, ''et al'' |title=Paracetamol plus ibuprofen for the treatment of fever in children (PITCH): randomised controlled trial |journal=BMJ |volume=337 |issue= |pages=a1302 |year=2008 |pmid=18765450 |pmc=2528896 |doi= |url=http://bmj.com/cgi/pmidlookup?view=long&pmid=18765450 |issn=}}</ref> | |||
== Toxicity and drug interactions == | == Toxicity and drug interactions == | ||
It may cause liver, blood cell, and kidney damage in a limited number of people. | While it is generally safe and effective, the margin between a safe and toxic dosage is narrower than once believed. In particular, overdoses are dangerous to the liver, once to be the case only in patients with alcohol-induced hepatic damage. While not yet a firm recommendation, there is increasing sentiment that patients taking it should not drink any alcohol while being treated. | ||
It may cause liver, blood cell, and kidney damage in a limited number of people. Alcohol intake increases its liver toxicity. The toxic effects of acetaminophen are due to a minor metabolite [[N-acetyl-p-benzo-quinone imine]], which reacts with [[sulfhydryl]] groups. At usual doses, it is detoxified by combining with [[glutathione]] to produce a non-toxic conjugate that gets excreted by the kidneys. | |||
The anticoagulation effects of [[acenocoumarol]], [[anisindione]], [[dicumarol]] and [[warfarin]] are increased when taken with acetaminophen. Increased liver toxicity occurs when used in combination with [[imatinib]], [[isoniazid]] or [[alcohol]]. | The anticoagulation effects of [[acenocoumarol]], [[anisindione]], [[dicumarol]] and [[warfarin]] are increased when taken with acetaminophen. Increased liver toxicity occurs when used in combination with [[imatinib]], [[isoniazid]] or [[alcohol]]. | ||
One third of patients taking a full | One third of patients taking a full dose (1 gram four times a day) may have their [[liver function tests]] rise to three times the upper limit of normal.<ref name="pmid16820551">{{cite journal |author=Watkins PB, Kaplowitz N, Slattery JT, ''et al'' |title=Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial |journal=JAMA |volume=296 |issue=1 |pages=87–93 |year=2006 |pmid=16820551 |doi=10.1001/jama.296.1.87}}</ref> | ||
==Dosage== | |||
The Food and Drug Administration may reduce the recommended dose to 650 milligrams per dose and no more than 3250 milligrams per day.<ref>Anonymous (2009) [http://www.fda.gov/ohrms/dockets/ac/09/briefing/2009-4429b1-01-FDA.pdf Acetaminophen Overdose and Liver Injury — Background and Options for Reducing Injury]</ref><ref name="urlThe Associated Press: FDA group recommends acetaminophen liver warnings">{{cite web |url=http://www.google.com/hostednews/ap/article/ALeqM5iIHiPgqCwdf8_--09SfBQFC4HD4wD98EREVG1 |title=The Associated Press: FDA group recommends acetaminophen liver warnings | |accessdate=2009-05-29}}</ref> | |||
==References== | ==References== | ||
{{reflist|2}} | |||
== External links == | == External links == | ||
* {{CZMed}} | * {{CZMed}} | ||
[[Category:Flagged for Review]][[Category:Suggestion Bot Tag]] | |||
Latest revision as of 06:00, 6 July 2024
Acetaminophen, also widely called acetaminofen, paracetamol or paracetanol, is an analgesic and antipyretic drug widely used for the treatment of headaches, fever and other minor aches and pains. Many cold and flu medications and some prescription analgesics contain acetaminophen. Although it is sold under hundreds of names, it is popularly known as Tylenol®.
The drug has long been considered especially safe, and replaced aspirin for many over-the-counter uses. It does not interfere with clotting mechanisms and increase bleeding tendency, and does not produce Reye's Syndrome in children. Nevertheless, suspicions arose that it could cause liver failure in heavy users of alcohol, but more data suggests there is a more general risk to the liver. In July 2009, an advisory committee to the Food and Drug Administration recommended that the maximum dose be reduced to 650 milligrams, from 1000 milligrams in current "extra strength" preparations. [1]
It has no mood altering effects and is not addictive although it can be combined with opioid analgesics which have these effects such as oxycodone or hydrocodone with the brand names of Percocet and Vicodin respectively. These combinations do offer some synergistic pain control, but that is not the primary purpose. Indeed, some prescribers may recommend that before increasing opioid dose, a second 300-375mg acetaminophen be taken with the combined tablet.
When the other drugs contain opioid analgesics, the primary purpose is to keep the oral dose from being diverted to recreational injection. The combination also has some therapeutic sense, because acetaminophen and opioids affect different mechanisms of pain. Unfortunately, there have been cases where raising the combined-tablet dose, usually to provide more opioid and often under medical orders, inadvertently produced acetaminophen toxicity. The FDA Advisory committee recommended, with a 20 to 17 vote, that prescription products that combine acetaminophen with other medications should be eliminated.[1] This does not affect over-the-counter cold products that combine acetaminophen with such other agents as decongestants and cough supressants, but addresses the situation when the patient might try to increase pain relief with what would be a safe additional opioid dosage, but overdose with acetaminophen. There is little reason to take higher dose of a cold medication.
Pharmacology
Mechanism of action
Acetaminophen inhibits cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) indirectly through a hypothesized yet unknown enzyme called COX-3, in the central nervous system and endothelial cells and thus suppresses the synthesis of prostaglandin and heightens the pain threshold. However, it does not inhibit COX enzymes in the peripheral tissues, and thus has no peripheral anti-inflammatory effects.
Metabolism
Glucuronosyltransferase is part of the phase II drug metabolism of acetaminophen.[2]
Effectiveness
Analgesia
Acetaminophen one gram orally four times a day had similar efficacy to ibuprofen in reducing pain in randomized controlled trial of patients with mild to moderate osteoarthritis or the hip or knee.[3]
"Diclofenac and paracetamol had the same effect on pain reduction of ankle sprains but more acute ankle edema was present in patients who were treated with diclofenac than in patients who were treated with paracetamol"according to a randomized controlled trial. [4]
Intravenous acetaminophen one gram was as effective as morphine 0.1 mg/kg for renal colic.[5]
Combination therapy
According to a systematic review sponsored by industry, combining acetaminophen with Non-steroidal anti-inflammatory agents may help treatment of posteroperative pain.[6]
For lumbalgia, acetaminophen one gram orally four times a day combined with diclofenac, a non-steroidal anti-inflammatory agent, was not better than acetaminophen alone in a randomized controlled trial.[7]
Acetaminophen has been combined with ibuprofen with uncertain results.[8]
Fever
For reducing fever, acetaminophen combined with ibuprofen may be better than either drug alone according to a randomized controlled trial.[9]
Toxicity and drug interactions
While it is generally safe and effective, the margin between a safe and toxic dosage is narrower than once believed. In particular, overdoses are dangerous to the liver, once to be the case only in patients with alcohol-induced hepatic damage. While not yet a firm recommendation, there is increasing sentiment that patients taking it should not drink any alcohol while being treated.
It may cause liver, blood cell, and kidney damage in a limited number of people. Alcohol intake increases its liver toxicity. The toxic effects of acetaminophen are due to a minor metabolite N-acetyl-p-benzo-quinone imine, which reacts with sulfhydryl groups. At usual doses, it is detoxified by combining with glutathione to produce a non-toxic conjugate that gets excreted by the kidneys.
The anticoagulation effects of acenocoumarol, anisindione, dicumarol and warfarin are increased when taken with acetaminophen. Increased liver toxicity occurs when used in combination with imatinib, isoniazid or alcohol.
One third of patients taking a full dose (1 gram four times a day) may have their liver function tests rise to three times the upper limit of normal.[10]
Dosage
The Food and Drug Administration may reduce the recommended dose to 650 milligrams per dose and no more than 3250 milligrams per day.[11][12]
References
- ↑ 1.0 1.1 Kathryn Foxhall, "FDA May Restrict Acetaminophen: Advisers Tell the Agency to Lower Over-the-Counter Dose of Popular Pain Drug", WebMD Health News
- ↑ de Wildt SN, Kearns GL, Leeder JS, van den Anker JN (1999). "Glucuronidation in humans. Pharmacogenetic and developmental aspects.". Clin Pharmacokinet 36 (6): 439-52. PMID 10427468.
- ↑ Bradley JD, Brandt KD, Katz BP, Kalasinski LA, Ryan SI (1991). "Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee". N. Engl. J. Med. 325 (2): 87–91. PMID 2052056. [e]
- ↑ Lyrtzis C, Natsis K, Papadopoulos C, Noussios G, Papathanasiou E (2011). "Efficacy of paracetamol versus diclofenac for Grade II ankle sprains.". Foot Ankle Int 32 (6): 571-5. DOI:10.3113/FAI.2011.0571. PMID 21733417. Research Blogging.
- ↑ Bektas F, Eken C, Karadeniz O, Goksu E, Cubuk M, Cete Y (2009). "Intravenous paracetamol or morphine for the treatment of renal colic: a randomized, placebo-controlled trial.". Ann Emerg Med 54 (4): 568-74. DOI:10.1016/j.annemergmed.2009.06.501. PMID 19647342. Research Blogging.
- ↑ Ong CK, Seymour RA, Lirk P, Merry AF (2010). "Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain.". Anesth Analg 110 (4): 1170-9. DOI:10.1213/ANE.0b013e3181cf9281. PMID 20142348. Research Blogging.
- ↑ Hancock MJ, Maher CG, Latimer J, et al (2007). "Assessment of diclofenac or spinal manipulative therapy, or both, in addition to recommended first-line treatment for acute low back pain: a randomised controlled trial". Lancet 370 (9599): 1638–43. DOI:10.1016/S0140-6736(07)61686-9. PMID 17993364. Research Blogging.
- ↑ Doherty M, Hawkey C, Goulder M, Gibb I, Hill N, Aspley S et al. (2011). "A randomised controlled trial of ibuprofen, paracetamol or a combination tablet of ibuprofen/paracetamol in community-derived people with knee pain.". Ann Rheum Dis 70 (9): 1534-41. DOI:10.1136/ard.2011.154047. PMID 21804100. Research Blogging.
- ↑ Hay AD, Costelloe C, Redmond NM, et al (2008). "Paracetamol plus ibuprofen for the treatment of fever in children (PITCH): randomised controlled trial". BMJ 337: a1302. PMID 18765450. PMC 2528896. [e]
- ↑ Watkins PB, Kaplowitz N, Slattery JT, et al (2006). "Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial". JAMA 296 (1): 87–93. DOI:10.1001/jama.296.1.87. PMID 16820551. Research Blogging.
- ↑ Anonymous (2009) Acetaminophen Overdose and Liver Injury — Background and Options for Reducing Injury
- ↑ The Associated Press: FDA group recommends acetaminophen liver warnings. Retrieved on 2009-05-29.
External links
- The most up-to-date information about Acetaminophen and other drugs can be found at the following sites.
- Acetaminophen - FDA approved drug information (drug label) from DailyMed (U.S. National Library of Medicine).
- Acetaminophen - Drug information for consumers from MedlinePlus (U.S. National Library of Medicine).
- Acetaminophen - Detailed information from DrugBank.