Shigella dysenteriae: Difference between revisions
imported>Walter Martinez |
imported>John J. Dennehy No edit summary |
||
| Line 1: | Line 1: | ||
{{subpages}} | {{subpages}} | ||
{{Taxobox | {{Taxobox | ||
| color = gray | | color = gray | ||
Revision as of 08:33, 19 May 2008
| Scientific classification | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
| Binomial name | ||||||||||||||
| Shigella dysenteriae |
Description and significance
Shigella dysenteriae was discovered in 1896 by the Japanese microbiologist Kiyoshi Shiga, which the genus was named after. It was the first in the species to be discover, and now they are three others that share the genus which include boydii, flexneri, and sonnei.[1] Shigella dysenteriae is gram-negative. Shigella dysenteriae are not capsualted, rod (bacillus) shaped, non-motile, non-spore-forming, facultative anaerobic bacteria.[1] The bacteria is able to survive contaminated environments as well as the acidity of the human gastro-intestinal tract. Shigella dysenteriae is important because it can pose a public health threat, especially in underdeveloped countries. The accumulation of bacterial Shigella dysenteriae in a host causes a condition known as shigellosis. If left untreated in a host, the infection can be lethal.
Genome structure
Shigella dysenteriae has the smallest genome out of the genus Shigella, which contains three other species. It's genome consists of a single circular chromosome and 4,369,232 base pairs.[3] It carries an invasion-associated plasmid which contains genes that code for the invasion of the epithelial cells and the production of Shiga toxin.[4] Shigella dysenteriae(bacillary dysentery), Historique.net: Infectious Disease</ref> The Shiga toxin is a potent A-B type toxin with 1-A and 5-B subunits. B subunits bind to the cell and inject the A-subunit. By cleaving a specific adenine residue from the 28S ribosomal RNA in the 60S ribosome, the toxin inhibits protein synthesis, causing cell death.[1]
Cell structure and metabolism
Describe any interesting features and/or cell structures; how it gains energy; what important molecules it produces
Shigella dysenteriae ferments glucose via mixed acid fermentation, however it does not produce any gas. It does not produce H2S, phenylalaninedeaminase or urease and does not use citrate as a sole carbon source.
Shiga Toxin
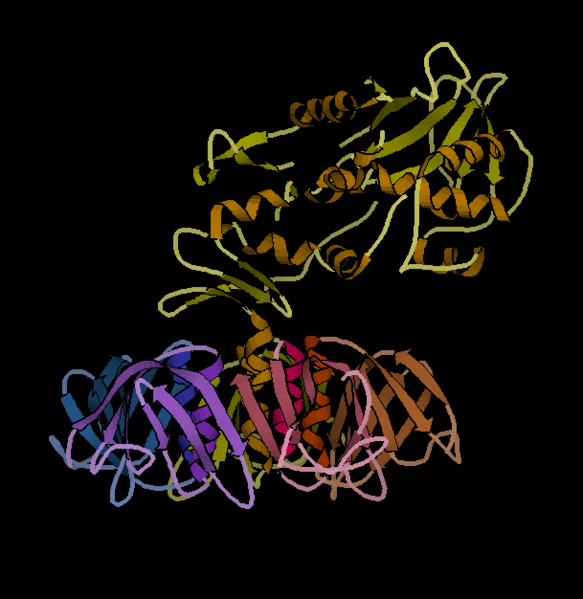 This is an image showing the crystalline structure of Shiga toxin. The bottom represents the beta subunits and the top represents the alpha subunits.
This is an image showing the crystalline structure of Shiga toxin. The bottom represents the beta subunits and the top represents the alpha subunits.
Shigella dysenteriae, produces Shiga toxin, which is used to infect host cells. Shiga toxin has a cytotoxic effect on intestinal epithelial cells.[5] Shiga toxin has a molecular weight of 68,000 daltons. The structure of the toxin is comprised of two types of subunits, alpha subunits and beta subunits. Beta subunits are responsible for binding to the host cell, whereas alpha subunits are responsible for poisoning the host cell. [1]
Shiga Toxin Mechanism
Shiga toxin attacks the surface of blood vessels inside the gastro-intestinal tract. The beta subunits of the Shiga toxin bind to the host cell. The alpha subunits are then injected into the cell, and these subunits work inhibit protein synthesis by deactivating the ribosomes. This eventually leads to the death of the cell, and hemmorrhage of the surface whcich it binds to. This accounts for the blood seen in the diarrhea. The toxin not only affect the digestive tract, but it attacks major structures associated with the kidneys function. The attack on these structures leads to kidney failure and the development of Hemolytic Uremic Syndrome.[1]
Ecology
Describe any interactions with other organisms (included eukaryotes), contributions to the environment, effect on environment, etc.
The only organisms that Shigella dysenteriae interacts with are humans, but other primates as well, and flies. Humans act as hosts for infection, which leads to bacillary dysentery. Flies can act as means of transportation for the bacteria, spreading it to other hosts.
Shigella dysenteriae can survive in faecally contaminated materials which can include water, foods, and other materials. It can be transmitted by person to person contact. It is generally transmitted with the ingestion of water and food contaminated with the bacteria. It can cause foodborne or waterborne epidemics. Water may become contaminated even if someone who has Shigellosis swims in it. Crops can be contaminated with the bacteria if they are watered with contaminated water. This will cause major problems if these contaminated crops are then distributed over a large region, exposing anyone who eats the crops to infection. Epidemics are more likely in poorer countries without adequate sanitation and water treatment systems.
Pathology
How does this organism cause disease? Human, animal, plant hosts? Virulence factors, as well as patient symptoms.
Shigella dysenteriae causes shigellosis (bacillary dysentery) in humans. It's also known to cause dysentery in other primates, but not in other animals. The infection can be caused by as little as 10 bacterial cells, whereas as other bacteria requires millions on cells for infection. This is due to the potency of the Shiga toxin. The infection begins with the bacteria entering the gastro-intestinal tract attaching itself to the intestinal wall. The bacteria invades the host cell injecting its Shiga toxin inside. This results in the degeneration of of the surface, causing blood leakage. Attachment of the Shiga toxin to the surface cells of the intestine prevents these cells from absorbing nutrients and water, which may lead to dehydration.[1]
The Shiga toxin has three effects on the human body, which include an neurotoxic, enterotoxic,and cytotoxic. Neurotoxic effects refer to fever and abdominal pains. Enterotoxic effects refer to the blocking of absorption in the intestine by attaching itself to the receptors in the intestine. Cytotoxic effects refer to the invasion of the the Shiga toxin on the epithelial cells. The beta subunits of the Shiga toxin binds to the glycolipid of the host cell, injecting alpha subunits via endocytosis. The alpha subunits attacks the ribosomes, deactivating the 60S ribosomal unit responsible for protein synthesis. This eventually leads to the death of the cell, damage to the intestinal lining and hemorrhage.
Common symptoms of bacillary dysentery include acute bloody diarrhea, abdominal pains and cramps, fever, vomiting, dehydration, and tenesmus. A more severe infection can lead to more severe complications such as hemolytic uremic syndrome, which develops in 5 to 10 percent of patients. Mortality from hemolytic uremic syndrome approaches 5 percent, but up to 30 percent of patients who survive have chronic renal disease.[5] Patients, in more severe cases, can also suffer from inflammatory colitis.
Shigellosis can resolve on its own in several days, but in smaller children and people with weak immune systems, the infection can be more severe, resulting in hospitalization or death. Once a person has become infected, they are not likely to get infected with the particular strain again, due to the bodies ability to produce antibodies. However, they can be reinfected by other strains of Shigella dysenteriae. Treatment includes the application of antibiotics. The antibiotics will kill the bacteria inside the gastrointerstinal tract, shortening its lifespan and therefore shortening the course of the infection. Some anitmicrobial agents used to treat bacillary desentery include, ciprofloxacin, ampicillin, trimethoprim-sulfamethoaxzole, and nalidixic acid. Other medication is used to treat other effect of the dysentery such as dehydration.
Current Research
Enter summaries of the most recent research here--at least three required
Recent studies have shown that Shigella dysenteriae, as well as other species within the genus, are becoming significantly more resistance to antibiotics in the United States. This resistance has made cases of infection by Shigella dysenteriae more difficult to treat, especially in children. Shigella are becoming more resistant to treatments which use ampicillin and trimethoprim-sulfamethoxazole (TMP-SMX). Shigella isolates were surveyed over a period of four years, and the there was a common trend in increasing rates of resistance to these animicrobial agents. Shigella dysenteriae isolates are also developing a resistance to nalidixic acid. It was also found that these resistances were not limited to the United states. Shigella dysenteriae isolates are becoming more resistant to antimicrobial agents in other parts of the world as well.[8]
It has been found that Shigella dysenteriae's virulence is regulated by RyhB suppression. The virulence genes that are being repressed by RyhB includes genes which code for the secretion apparatus, its effectors and its chaperones. It was found that the virulence suppression was occurs by the RyhB dependent repression of the transcriptional activator VirB which lead a reduction in expression of genes within the VirB region. Several tests were conducted such as microarray analysis, secreted protein analysis and Polymerase Chain Reaction. It was concluded that RyhB represses the expression of several genes within VirB region, which in turn, suppresses plaque formation by inhibiting the ability of Shigella dysenteriae to invade eukaryotic cells. There is a direct relationship between plaque formation and RyhB expression. It was then further determined that since RyhB is iron-responsive, iron, therefore contributes to the regulation of virulence within Shigella dysenteriae.[9]
There has been one case of Shigellosis discovered in which the patient suffered from septic shock and convulsions, which is an unusual side effect of the infection. The patient had the usual symptoms of bloody diarhhea, tenesmus and fever. The patient also suffered from abnormal body movement and did not respond to the initial treatments with trimethoprim-sulphamethoxazole, which suggests that the particular strain of the infection was resistant to the antibiotic. Various tests, such as blood films, stool microscopy, stool culture and cerebrospinal fluid cultures, were conducted to determine the cause of this case of Shigellosis, but all came up negative. Finally, a tests was done on the blood culture and after a few days colony growth was observed and Shigella dysenteriae was isolated. Sensitivity test were then conducted on the bacteria. It was determined that the bacteria was resistant to chloramphenicol, TMP-SMX, ampicillin, and tetracycline, but sensitive to ciprofloxacin and gentamycin. The patient was given medication for the septic shock, which subsided soon afterward. However, the patient died soon after. It was thought that the septic shock was a result of the build up of Shiga toxin produced by the bacteria. It was concluded that when not appropriately and promptly treated, these infections can lead to more serious and lethal side effects.[10]
References
1. Swapan Kumar Niyogi "Shigellosis". "The Journal of Microbiology". 43(2),133-1430, 2005,
3. Shigella dysenteriae, KEGG Genome
4. Shigella dysenteriae(bacillary dysentery), Historique.net: Infectious Disease