Adipocyte
The adipocyte, a cell type located in adipose tissue, stores excess fat and makes it available on demand to the body system for use as energy. Adipocytes can also secrete signaling messengers, called adipokines. Adipose tissue — which consists of other cell types besides adipocytes — operates as an endocrine organ, secreting more than 50 known adipokines.[1] There are two different types of adipose tissue, white and brown. White adipose tissue (WAT) is the fat storage tissue and brown adipose tissue (BAT) produces heat. BAT is sometimes popularly called ‘baby fat’ as it is present in babies but converts to WAT in adulthood. This conversion is performed by mitochondrial uncoupling protein 1 (UCP1), which is activated by the diet, in the mitochondria. Mice that are genetically made to express UCP1 in their WAT become obesity resistant, and this has sparked interest in a possible treatment for obesity, by identifying what causes the UCP1 to stop working and so convert BAT to WAT, and then finding a way to stop that so that excess energy is released as heat rather than stored in WAT resulting in obesity.
Pioneering studies
Fat cells were first considered to be able to sense energy demands and signal to decrease food intake in the 1950’s. However it was not confirmed until 1973, when Coleman, in animal experiments involving parabiosis, provided evidence that a circulating factor existed that signalled information about the body's energy requirements. This idea gained little attention until Siiteri in 1987 examined the role of obesity in cancers of the reproductive tract and found that adipocytes secreted the hormone oestrogen which is implicated in breast and endometrial cancers. Oestrogen is produced by the aromatase enzyme which is present in many tissues including adipose tissue. The production of oestrogen is accelerated in people that are obese, as more adipose tissue means more oestrogens and this is correlated with a higher incidence of cancers in the reproductive tract in obese individuals. Another prospect which supported the adipocyte as a regulator of energy stores came when adipsin, a serine protease, was also discovered to be secreted by adipocytes, and has since been found to be deficient in some animal models of obesity.
Obesity brings with it associated complications including cardiovascular problems, some cancers and type 2 diabetes mellitus. As cases of obesity are increasing in adults, so are cases of diabetes but perhaps more alarmingly is the increase in obesity related diabetes in children. The reason for the strong relationship between obesity and type 2 diabetes mellitus is still largely unknown, but it has been proposed that the physiology of adipocytes may hold the key.
Resistin
In 2001, an article in the Washington Post read, ‘Hormone may be key to diabetes’ [2]. The hormone was resistin, secreted from adipocytes of white adipose tissue, and it had been found to be involved in the emergence of T2DM. Resistin blood serum levels were significantly increased in cases of obesity and it was found to interfere with the actions of insulin and with glucose tolerance, causing insulin resistance in mice. This was also supported by research showing that deliberately induced diabetes, caused by provision of a high fat diet, caused obesity and elevated resistin levels in mice. These effects could be reversed by administration of a resistin antibody [3]. This discovery sparked excitement, as resistin appeared to be a candidate for the missing link between obesity and T2DM. However studies in humans showed no significant differences between blood serum resistin levels in lean and obese people and no differences between serum resistin levels in healthy and diabetic people. These conclusions imply that resistin does not play a role in obesity related diabetes and does not seem to be governed by adiposity. The differences between humans and mice may be due to differences in energy metabolism and in genetic differences between the species, as the mouse resistin gene is not identical to the human gene, only showing 59% homology (Lee et al. 2003).
More recent studies have found supernormal plasma concentrations of resistin in humans (South Koreans) with type 2 diabetes[4] though the studies yielded no insight into the role of the higher resistin levels. They were not related to gender or degree of obesity or insulin resistance. Saudi Arabians with diabetes mellitus type 2 also have increased plasma resistin levels when assessed for the presence of the so-called metabolic syndrome, an array of risk factors for cardiovascular disease (e.g., obesity in and around the abdomen; increased blood levels of those lipids that predispose to atherosclerosis; impaired ability to use insulin or blood sugar; indications of inflammation in the body) [5]. That association of high resistin levels and the metabolic syndrome has been confirmed by other investigators (Norata et al., 2007). In a Turkish study group, investigators found that one specific form of the resistin gene (polymorphism) associated with insulin resistance and obesity in patients with T2DM [6]
Taken together, those findings link resistin and diabetes mellitus type 2, but shed no light on the functional role of resistin in humans. Because in addition to adipocytes, cells involved in immunity and inflammation produce resistin, the link between resistin and diabetes might relate to inflammatory reactions in T2DM, an area needing further investigation [7]; [8]
In 879 non-diabetic humans, Reilly et al. tested for an association between plasma resistin concentrations and metabolic and inflammatory markers, including coronary artery calcification as an index of atherosclerosis, finding positive associations with inflammatory markers (soluble tumor necrosis factor-receptor-2; interleukin-6; and lipoprotein-associated phospholipase A2. They found no association with insulin resistance, but did with coronary calcification after appropriate justments for confounders. They concluded: "Plasma resistin levels are correlated with markers of inflammation and are predictive of coronary atherosclerosis in humans, independent of CRP [C-reactive protein, a marker of inflammation]. Resistin may represent a novel link between metabolic signals, inflammation, and atherosclerosis."[9]
Visfatin
Another adipokine implicated in the obesity-diabetes saga is the molecule visfatin. Visfatin is secreted by visceral fat and has glucose-lowering effects similar to those of insulin. Visfatin and insulin stimulate muscle and adipose cells to take up glucose and restrain glucose release from hepatocytes. [10] However, visfatin is unlike insulin in that its levels are constant regardless of food intake whereas insulin levels change depending on the feeding state. Visfatin also has significantly lower intracellular levels than insulin but interestingly it acts on the insulin receptor but not competitively. This may mean that visfatin is a mimetic of insulin, but its levels are low enough so that it does not interfere with the actions of insulin.
So fat cells are no longer considered to be just a fat store, but are dynamic cells that work to maintain the body's energy homeostasis. Many other molecules have been identified that are secreted by adipocytes, some those not involved in energy homeostasis eg. the cytokines.
Leptin
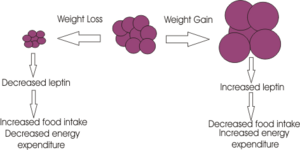
Probably the biggest breakthrough for the study of appetite regulation came in 1994 when the molecular geneticist Jeffrey Friedman discovered the adiposity signal leptin. Using the ob/ob mice which were thought to lack a satiety signal, Friedman and colleagues found that 'ob' codes for a gene which they called leptin, from the Greek ‘leptos’ meaning thin. Mice deficient in this gene are morbidly obese and this obesity can be reversed by giving the mice leptin. The leptin receptor was found in 1995 and is a member of the cytokine receptor family.[11]
Leptin is a signalling molecule released from adipocyte cells to signal regarding adiposity levels. It is secreted into the blood, secretion proportional to body fat, where it travels to the brain causing a decrease in appetite through acting on specific neurones in the brain.[12]
Unsurprisingly there was huge media interest in leptin as a possible treatment for obesity, and the biotechnology company Amgen paid $20 million to license leptin. However the results of clinical trials on obese people were disappointing, with very few of the participants losing weight. It appeared that most people were not obese because of a deficiency in leptin, but were just unable to respond to it; they had more fat cells and so more circulating leptin and as a result, reduced sensitivity of the leptin receptor. The failure of the trial, however, overshadowed the fact that about 30% of the subjects lost weight and so may have low circulating levels of leptin. Potentially these people might benefit from leptin therapy. The task now though is to determine those people that have a lower circulating level of leptin.
The use of leptin as a drug has proved valuable in the disease lipodystrophy and in people who have a defective leptin gene and so are constantly hungry.
Leptin inhibits food intake by acting in the appetite control centres of the brain. Leptin receptor mRNA is found primarily in the hypothalamic arcuate nucleus, ventromedial nuclei and dorsomedial hypothalamic nuclei, regions that are known to be involved in appetite control.
The weight loss caused by leptin seems to arise because of two effects;
1. Inhibiting appetite through its actions on the appetite-stimulating neuropeptide Y neurones and the appetite-inhibiting proopiomelanocortin (POMC) neurons, located in the hypothalamic arcuate nucleus. Leptin inhibits the NPY neurons,causing a decrease in the release of the inhibitory neurotransmitter GABA (which is synthesised by the NPY neurons). This "disinhibits" the POMC neurons which increase their firing rate leading to the release of alpha MSH – a product of POMC which is a potent inhibitor of appetite. Leptin also acts directly on the POMC neurons.
2. Leptin also increases energy expenditure by increasing body temperature and oxygen consumption
As yet it is still unknown how exactly leptin exerts its inhibitory effects on feeding behaviour. It acts on the JAK/STAT pathway, effecting gene transcription and other cellular signalling pathways but a definitive mode of action has not been found; leptin's mode of action probably involves several different signalling pathways.
Leptin is synthesised in many other tissues including the stomach, ovary, placenta and liver and its receptors are also located in a diverse range of tissues. It plays a role in many other physiological functions such as reproduction, where levels of leptin appear to dictate the commencement of menstruation and in foetal development where there is a surge in leptin levels in the first week of life, which does not correspond to a decrease in food intake but is thought to be a developmental signal. During development, mice deficient in leptin have disruptions in the arcuate nucleus neural projections, but not other hypothalamic projections, and these effects can be reversed upon leptin treatment.
Leptin’s main function is still under consideration as it also plays a role in many other physiological processes. For example it can be thought of as a signal informing the body when it has sufficient fat to accommodate an ‘expensive’ physiological function like reproduction. Leptin therefore appears to protect the body against starvation by only allowing energy dense processes to occur when the body is sufficiently ready. Its primary role is complex, is it a satiety signal to prevent overeating or an evolutionarily efficient signal protecting against starvation?
Adiponectin
Adiponectin alters insulin receptor function, diminishes the action of insulin in the liver, alters the metabolism of free fatty acids by liver cells, and protects against inflammation. Adults and children (humans) who have non-alcoholic fatty liver disease (NAFLD) show decreased plasma concentrations of adiponectin. Inasmuch as insulin resistance in the liver, and hyperinsulinemia, feature in NAFLD, those finding suggest a link between fatty liver and insulin resistance perhaps in part to reduced adiponectin. NAFLD also features elevated levels of leptin, an adipokine that reduces appetite but also interferes with insulin action in the brain.[13] [14] [15] [16] [17] [18]
Adiponectin exhibits the following actions:[19] [20] [21] [22] [23] [24] [25] [26]
- Perhaps by increasing fatty acid oxidation, a smaller increase in plasma FFA occurs after a high fat meal;
- By enhancing lipid metabolism, insulin sensitivity improves;
- Reduced glucose production by the liver;
- Plasma concentrations associate inversely with endogenous glucose production.
In patients who have had an acute myocardial infarction, the risk of subsequent major adverse cardiovascular events is lowest in patients with the highest plasma concentrations of adiponectin. [27]
A complex incompletly elucidated relationship exists between adipose tissue cytokines and bone metabolism. Some workers find that in postmenopausal women plasma adiponectin concentrations associate inversely with bone mineral density.[28]
Table of molecules released by adipose tissue
Adipose Tissue |
Adipose Tissue | |
| Acylation stimulating protein[29] [30] | ||
| Adiponectin[31] | ||
| Angiotensinogen [32] [33] [34] [35] | ||
| Atrial Natriuretic Peptide | ||
| Cholesteryl-ester transferase | ||
| Estrogens | ||
| Free Fatty Acids/Glycerol | ||
| IGF-binding protein 3 (IGFBP3) | ||
| Insulin-like growth factor-I | ||
| Interleukin-6 | ||
| Leptin | ||
| Lipoprotein lipase | ||
| Monobutyrin | ||
| Plasminogen Activator Inhibitor - factor 1 | ||
| Resistin | ||
| Retinol binding protein-4 | ||
| Tumor necrosis factor-a | ||
| Visfatin | ||
| Adapted from Garrutti et al.[36] and modified by Citizendium editors. | ||
Notes
- ↑ Note: Adipokines influence such processes as inflammation, control of appetite and energy balance, sensitivity to insulin, the metabolism of fats, and the growth of new blood vessels.
- ↑ Washington Post, Jan 18th, 2001
- ↑ Steppan et al. (2001) The hormone resisten links obesity to diabetes. Nature 409:307-12 -First discovered resistin as a link between obesity and diabetes.
- ↑ Youn BS et al. (2004) Plasma resistin concentrations measured by enzyme-linked immunosorbent assay using a newly developed monoclonal antibody are elevated in individuals with type 2 diabetes mellitus. J Clin Endocrinol Metab 89:150-6 PMID 14715842.
- ↑ Al-Daghri NM et al. (2007) Adipocytokine profile of type 2 diabetics in metabolic syndrome as defined by various criteria. Diabetes Metab Res Rev; (Article online in advance of print) http://www3.interscience.wiley.com/cgi-bin/fulltext/114297091/HTMLSTART
- ↑ Duman BS et al. (2007) Association of resistin gene 3'-untranslated region EX4-44G-->A polymorphism with obesity- and insulin-related phenotypes in Turkish type 2 diabetes patients. Rev Diabet Stud 4:49-55
- ↑ Lago F et al. (2007) The emerging role of adipokines as mediators of inflammation and immune responses. Cytokine Growth Factor Rev 18:313-25.
- ↑ Anderson PD et al. (2007) Innate immunity modulates adipokines in humans. J Clin Endocrinol Metab 92:2272-9
- ↑ Reilly MP et al. (2005) Resistin is an inflammatory marker of atherosclerosis in humans. Circulation 111:932-9
- ↑ Fukuhara et al. (2005) Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science 307:426-30 - Discovery of another protein secreted from fat that may provide the link between obesity and diabetes
- ↑ Zhang et al. (1994) Positional cloning of the mouse obese gene and its human homologue. Nature 372:425-32 - these authors first identified leptin
- ↑ Schwartz et al. (2000) Central nervous system control of food intake. Nature 404:661-71 - detailing the effects of leptin on molecular pathways in the brain.
- ↑ Roberts EA. (2007) Pediatric nonalcoholic fatty liver disease (NAFLD): a "growing" problem?" J Hepatol 46:1133-42.
- ↑ Stefan N, Hennige AM, Staiger H, Machann J, Schick F, Krobe SM, et al. (2006) a2-Heremans-Schmid Glycoprotein/Fetuin-A is associated with insulin resistance and fat accumulation in the liver in humans. Diabetes Care 29:853–857.
- ↑ Bugianesi E, Pagotto U, Manini R, Vanni E, Gastaldelli A, de Iasio R, et al.(2005) Plasma adiponectin in nonalcoholic fatty liver is related to hepatic insulin resistance and hepatic fat content, not to liver disease severity. J Clin Endocrinol Metab 90:3498–3504.
- ↑ Pagano C, Soardo G, Esposito W, Fallo F, Basan L, Donnini D, et al. (2005) Plasma adiponectin is decreased in nonalcoholic fatty liver disease. Eur J Endocrinol 152:113–118.
- ↑ Louthan MV, Barve S, McClain CJ, Joshi-Barve S. (2005) Decreased serum adiponectin: an early event in pediatric nonalcoholic fatty liver disease. J Pediatr 147:835–838.
- ↑ Gil-Campos M, Canete RR, Gil A. Adiponectin, the missing link in insulin resistance and obesity. Clin Nutr 23:963–974.
- ↑ Guerre-Millo M. (2007) Adiponectin: An update. Ddiabetes & Metaboism 34:12-18.
- ↑ Fruebis J., Tsao T.S., Javorschi S., Ebbets-Reed D., Erickson M.R., Yen F.T., et al. (2001) Proteolytic cleavage product of 30-kDa adipocyte complement-related protein increases fatty acid oxidation in muscle and causes weight loss in mice Proc Natl Acad Sci USA 98:2005-2010
- ↑ Yamauchi T., Kamon J., Waki H., Terauchi Y., Kubota N., Hara K., et al. (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7:941-946.
- ↑ Berg A.H., Combs T.P., Du X., Brownlee M., Scherer P.E. (2001) The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med 7:947-953.
- ↑ Combs T.P., Berg A.H., Obici S., Scherer P.E., Rossetti L. (2001) Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J Clin Invest 108:1875-1881.
- ↑ Bajaj M., Suraamornkul S., Piper P., Hardies L.J., Glass L., Cersosimo E., et al. (2004) Decreased plasma adiponectin concentrations are closely related to hepatic fat content and hepatic insulin resistance in pioglitazone-treated type 2 diabetic patients. J Clin Endocrinol Metab 89:200-206.
- ↑ Miyazaki Y., Mahankali A., Wajcberg E., Bajaj M., Mandarino L.J., DeFronzo R.A. (2004) Effect of pioglitazone on circulating adipocytokine levels and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab 89:4312-4319.
- ↑ Bugianesi E., Pagotto U., Manini R., Vanni E., Gastaldelli A., de Iasio R., et al. (2005) Plasma adiponectin in nonalcoholic fatty liver is related to hepatic insulin resistance and hepatic fat content, not to liver disease severity. J Clin Endocrinol Metab 90:3498-3504.
- ↑ Huang,S.S.; Huang,P.H.; Chen,Y.H.; Chiang,K.H.; Chen,J.W.; Lin,S.J. (2010) Association of Adiponectin with Future Cardiovascular Events in Patients After Acute Myocardial Infarction. J Atheroscler.Thromb. Advance Publication Online Feb. 2010.
- ↑ Wu N, et al. (2010) Relationships between serum adiponectin, leptin concentrations and bone mineral density, and bone biochemical markers in Chinese women. Clin Chim Acta In Press.
- ↑ Ahrén B, Havel PJ, PaciniG, Cianflone,K. (2003) [http:/dx.doi.org/10.1038/sj.ijo.0802369 Acylation stimulating protein stimulates insulin secretion.] International Journal of Obesity (2003) 27, 1037–1043.
- From Abstgract: Acylation stimulating protein (ASP) is a hormone produced by adipocytes and is of importance for the storage of energy as fat….ASP augments glucose-stimulated insulin secretion through a direct action on th islet beta cells….Stimulation of insulin secretion by ASP in vivo results in augmented glucose disposal. n on the islet beta cells.
- ↑ Schrauwen P, Hesselink MKC, Jain M, Cianflone K. (2005) Acylation-stimulating protein: effect of acute exercise and endurance training. International Journal of Obesity 29:632–638.
- From Abstract: Acylation-stimulating protein (ASP) is an adipocyte-derived protein that contributes to fatty acid clearance….Regular exercise training improves fatty acid handling….Short-term endurance training reduces baseline ASP levels….These data fit with the hypothesis that reduced ASP levels indicate improved ASP sensitivity
- ↑ Guerre-Millo M. (2008) Adiponectin: an update. Diabtese Metab 34:12-18. PMID 18069030.
- ↑ Karlsson C, Lindell K, Ottosson M, Sjostrom L, Carlsson B, Carlsson LM. (1998) Human adipose tissue expresses angiotensinogen and enzymes required for its conversion to angiotensin II. (Free Full-Text) J Clin Endocrinol. Metab 83:3925-9. PMID 9814470.
- From the Abstract: Angiotensin II regulates blood pressure and may affect adipogenesis and adipocyte metabolism. Angiotensin II is produced by cleavage of angiotensinogen by renin and angiotensin-converting enzyme in the circulation. In addition, angiotensin II may be produced in various tissues by enzymes of the renin-angiotensin system (RAS) or the nonrenin-angiotensin system (NRAS)….We conclude that human adipose tissue expresses angiotensinogen and enzymes of RAS and NRAS. This opens the possibility that angiotensinogen-derived peptides, produced in adipose tissue itself, may affect adipogenesis and play a role in the pathogenesis of obesity.
- ↑ Muller-Wieland D, Kotzka J, Knebel B, Krone W. (1998) Metabolic syndrome and hypertension: pathophysiology and molecular basis of insulin resistance. Basic Res. Cardiol. 93 Suppl 2:131-4. PMID 9833175.
- From the Abstract:Several recent studies indicate that type 2 diabetes, arterial hypertension, lipid disorders as well as visceral obesity are coronary risk factors which might belong to a syndrome which is caused by decreased insulin sensitivity with compensatory hyperinsulinaemia. More than 50% of patients with essential hypertension have some degree of insulin resistance, but in contrast to dyslipoproteinaemia and glucose intolerance the causal relation between insulin resistance and elevated arterial blood pressure appears not to be as evident. One explanation is that the link between blood pressure and insulin sensitivity might be mainly related to concomitant obesity. Accordingly, obesity can be associated with an increased activity of the sympathetic nervous system, elevated plasma levels of the vasoconstrictor endothelin-1, and decreased insulin-induced endothelium-dependent vasodilation. Furthermore, adipocytes can secrete vasogenic peptides, such as angiotensinogen. Since insulin resistance is a polygenic disorder, the two basic genetic approaches we follow is to identify genetic defects of insulin action in cells of patients with inherited syndromes of insulin resistance and to characterize molecular mechanisms of insulin regulated gene expression. The results show that insulin can affect the expression rate of various genes, e.g. involved in cholesterol and fatty acid metabolism, by modulating the activity of transcription factors coupled to the MAP kinase cascade and that a genetic postreceptor defect in these intracellular signaling pathways might have a pleiotropic effect on cell metabolism and clinical phenotype.
- ↑ Giacchetti G, Faloia E, Sardu C, Camilloni MA, Mariniello B, Gatti C, Garrapa GG, Guerrieri M, Mantero F. (2000) Gene expression of angiotensinogen in adipose tissue of obese patients. Int. J Obes. Relat Metab Disord. 24 Suppl 2:S142-S143. PMID 10997636.
- From the Abstract: Recently, the genes of components of the renin-angiotensin system (RAS), namely angiotensinogen (AGT), angiotensin converting enzyme and angiotensin II receptor have been described in adipose tissue. In animal models the angiotensinogen in adipose tissue has been implicated in the pathogenesis of metabolic alterations and hypertension associated with obesity…. [The] data suggest that angiotensinogen may be determinant of fat distribution and may be involved in the plurimetabolic syndrome of central obesity.
- ↑ Bulcao C, Ferreira SR, Giuffrida FM, Ribeiro-Filho FF. (2006) The new adipose tissue and adipocytokines. Curr. Diabetes Rev. 2:19-28. PMID 18220614.
- From the Abstract: Obesity is a well-known risk factor for the development of insulin resistance, type 2 diabetes, dyslipidemia, hypertension, and cardiovascular disease. Rather than the total amount of fat, central distribution of adipose tissue is very important in the pathophysiology of this constellation of abnormalities termed metabolic syndrome. Adipose tissue, regarded only as an energy storage organ until the last decade, is now known as the biggest endocrine organ of the human body. This tissue secretes a number of substances--adipocytokines--with multiple functions in metabolic profile and immunological process. Therefore, excessive fat mass may trigger metabolic and hemostatic disturbances as well as CVD. Adipocytokines may act locally or distally as inflammatory, immune or hormonal signalers. In this review we discuss visceral obesity, the potential mechanisms by which it would be related to insulin resistance, methods for its assessment and focus on the main adipocytokines expressed and secreted by the adipose tissue. Particularly, we review the role of adiponectin, leptin, resistin, angiotensinogen, TNF-alpha, and PAI-1, describing their impact on insulin resistance and cardiovascular risk, based on more recent findings in this area.
- ↑ Garrutti G, Cotecchia S, Giampetruzzi, Giorgino F, Giorgino R. (2008) Neuroendocrine Deregulation of Food Intake, Adipose Tissue and the Gastrointestinal System in Obesity and Metabolic Syndrome. (Free Full-Text) J Gastrointestin Liver Dis 17:193-198. PMID 18568142
References
Flier J et al. (1987) Severely imparied adipsin expression in genetic and acquired obesity. Science 237:405-408 - Realisation that the fat cell is more than just a fat storage molecule
Norata GD et al. (2007) Plasma resistin levels correlate with determinants of the metabolic syndrome. Eur J Endocrinol 156:279-84.