Venereal disease
Venereal diseases are infections spread through sexual contact. What is special about such diseases is the germs that cause them- these agents, whether they be bacteria, viruses, or other types of microorganisms, can only remain infectious if kept at the conditions that exist inside a living person. Unlike the virus that causes the common cold, once they leave the body's warm environment, with its supples of oxygen and nutrients and living cells, they cannot survive. The pathogens that cause venereal disease can infect solely by passing directly from one body into another, through living fluids. When the term, "venereal disease" was coined, in the 19th century, sexual activity was the only prolonged "intimate" means of sharing body fluids that occured with any regularity, except for the special case of mother and infant during pregnancy and at birth. Since that time, with the advent of blood transfusion, organ transplant, and groups of substance abusers who share hypodermic equipment for injecting drugs, some of the same fastidious organisms that could only survive transmission from an infected person to a new host through sexual contact now are also able to survive through these other forms of transport.
Some venereal diseases can be passed from an infected mother to her baby: either during pregnancy, birth, or through breastfeeding. This fact has changed the utility of breastfeeding in some areas, like sub-Saharan Africa, where the rate of HIV (which is transmitted in breast milk) is very high. It also had an influence on the social mores of Europe, where, after syphilis became epidemic in the 15th century, women warned their daughters about the dangers of marrying the wrong man, lest the children bring tragedy.
Sexually transmitted diseases (STD) include both the venereal diseases and other infections. These other kinds of infections can be spread in many ways, but are so likely to be transmitted by sexual contact with an infected person that they are included in the category. This article reviews the history and significance of the venereal diseases in human society.
Venereal disease of bacterial origin
Syphilis
"Worldwide, there are an estimated 12 million new syphilis cases every year, over 90% of which occur in developing countries."(reference for quote:Gaudio PA. Update on ocular syphilis. Current Opinion in Ophthalmology. 17(6):562-6, 2006 Dec. UI: 17065926). Since early syphilis is now curable with medical treatment, persistant cases are the result of either (1) the lack of available medical care (which accounts for the predominance of cases in the developing world), (2) medical negligence or misdiagnosis, or (3) the failure of the infected individual to seek medical attention or to complete recommended treatment. That failure generally occurs either because the individual does not understand that he or she may have an infection that requires treatment, or because of apathy towards self-care.
Syphilis in historical perspective
As far as recorded history is concerned, syphilis made its debut in 15th century Europe. Whether it came from the sailors returning from the new world, or from a new strain of a locally established organism (related to the spirochete of a similar species that causes yaws) is unknown. What is known is that "the great pox" began and, by the 17th century, epidemics of syphilis had not only spread through the population of Europe but had been carried by travelling Europeans to other areas of the world. In this early era of syphilis that disease was as devastating to the populations it infected as a later epidemic of a sexually transmitted illness, AIDS, has been. Until the discovery of antibiotics, the incidence and prevalence of syphilis rose dramatically after every war, beginning with the Neopolonic and ending with War World II. Public education and treatment with penicillin have both been important in changing this pattern.
In the pre-antibiotic era, when toxic heavy metal containing compounds were the only effective remedies for the dread venereal disease, syphilis, the standing joke among medical students was " one night on Venus and the rest of your life on Mercury". These compounds did kill the spirochete, and sometimes cured the syphilis infection, but also made the patient sick and sometimes caused life long side effects, whether or not the syphilis was cured.
By the middle of the 20th century, the treatment situation suddenly changed and syphilis became easily curable- at least in its early stages. Penicillin, along with sex education, changed the demographics of the disease. In the United States, because of "widespread screening and treatment by the Surgeon General Thomas Parran after the Second World War, reported cases of primary and secondary syphilis dropped to an all-time low in 1955." However, rates did rise again, and have shown a 10-year cycle of rising and falling in a fairly regular fashion.
"In North America and the developed countries of northern Europe, syphilis had become predominately a disease of homosexual men by the 1970s. During the late 1980s, there were renewed outbreaks of heterosexual and congenital syphilis in North America in the wake of the HIV epidemic."(George R Kinghorn Chapter 75 – Syphilis in Cohen & Powderly: Infectious Diseases, 2nd ed. copyright 2004). That epidemic ended, to be replaced, in terms of global infection, with a large increase in cases in Eastern Europe and parts of Asia. In the Soviet Union (1918–1992), public health, including sexually transmitted disease (STD) control, was carefully monitored, with rights of personal freedom and privacy secondary to the control of disease. These strict and enforced measures controlled syphilis in the USSR. The incidence of syphilis never exceeded 40 cases per 100,000 in St. Petersburg, during the soviet regime. The collapse of the USSR in the early 1990s caused not only a collapse of the syphilis control program, but a fundamental change in the economic, social, and psychologic makeup of life in Russia. This period marked the rise of a Russian syphilis epidemic.
Stages of syphilis
for more detailed and technical information see syphilis
Syphilis is an unusual infectious disease because this illness is qualitatively different at different stages of infection. There are 3 such stages, and the disease is accordingly named: primary, secondary, and tertiary syphilis. Without treatment, syphilis is marked by periods of acute symptoms, followed by latent periods. Those latent periods often delude the infected person into believing that whatever was wrong has now healed or passed, because most or all of the symptoms or signs that flared in the acute period disappear on their own. Despte that, the infection does not go away without treatment and the disease progresses from the first, to the second, and then to the third stage.
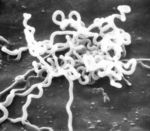
Although antibiotic treatment is effective for early syphilis, tertiary syphilis is not easily eradicated and is often associated with permanent damage, whether or not the infecting organisms can be completely banished from the body. In some ways, these features of syphilis are similar to another spirochete infection, one that is not venereal in nature but spread by the bite of infected ticks, Lyme disease. The spirochete that causes syphilis, Treponemum pallidum pallidum, is one of two subspecies of T. pallidum that causes human disease. T. pallidum can push its way through the unbroken mucosa of the genital tract and of the inner nose, lips, oral cavity, and throat, and can also enter the body through microscopic breaks in skin.

Early syphilis
Early syphilis includes both the primary and secondary stages. During this time the disease is easily passed to sexual contacts, and is also easily curative with the proper antibiotic treament. The signs and symptoms of early syphilis will go away by themselves without treatment, but the infection will not. Instead the disease will progress to the late stage in which treatment does not reliably produce a cure. For both selfish and altruistic reasons, a person who may possiby have syphilis is best tested for the infection as soon as possible. In many countries and regions within nations, such tests are carried out routinely during the prenatal care of pregnant women, and upon admission to the hospital or application for marriage licenses.
Primary syphilis
The lesions of primary syphilis do not appear immediately after the infection is contracted. The infecting organism, the spirochete T. pallidum enters the new host's body (either through intact mucosa or a small break in the skin) and then begins to reproduce in the superficial tissues near the entry site. After about two to six weeks from the that time, that area of skin or mucosa will show lesion or lesions: usually a painless nodule. The lesion of primary syphilis is called a chancre. This nodule, a round thickening of tissue, may ulcerate and appear to be an open wound, or the nodules may be multiple, in some cases, they have a wart-like appearance rather than appearing smooth. Physicans describe regional enlargement of lymph nodes that occurs along with the appearance of this primary lesion, but the lymph node enlargement is also painless - and may not be noticed by the afflicted person. Regional lymph nodes drain the part of the body that is infected with the primary chancre of syphilis and enlarge because they also become secondarily infected. Their location in the body depends on the location of the lesion. If the chancre is on the lip, the lymph nodes that enlarge will be in the neck. Chancres are usually on the genitals, and so, the enlarged lymph nodes are ordinarily in the groin ("inguinal adenopathy)". However, the primary lesion of syphilis can appear anywhere on the body that had an area that contacted the other person's reservoir of infection and allowed entry of the spirochete through a break in the skin. If that area was a finger, for example, the enlarged lymph nodes will be under the arm- the axillary lymph nodes.
Secondary syphilis

Late syphilis
Tertiary syphilis
The externally visible lesions of late (tertiary) syphilis is called a gumma. (reference:Nicholas L. Beerman H. Late syphilis: a review of some of the recent literature. American Journal of the Medical Sciences. 254(4):549-69, 1967 Oct. UI: 4862998)
Congenital syphilis
Although the great majority of cases of syphilis are contracted through sex, infants born to untreated mothers with either primary, secondary or tertiary syphilis may be infected. This type of syphilis is known as congenital syphilis, and it is a leading cause of stillbirths and death among newborns and young infants in many developing countries. In developed countries, blood tests for syphilis are a routine part of prenatal care.
The incidence of congenital syphilis" is a lower, but parallel, incidence of the infectious syphilis in females. In the USA, "the number of reported cases of congenital syphilis in infants 1 year of age was lowest (107 cases) in 1978, when infectious syphilis was most prevalent among homosexual and bisexual men. The dramatic increase in the incidence of primary and secondary syphilis among women from 1986 to 1990 resulted in a proportionate increase in the number of infants born with congenital syphilis—to 4424 infants in 1991. The incidence of early syphilis among women has declined since 1991, as has the number of reported cases of congenital syphilis in infants (with 529 cases in 2000). It is important to note that the case definition for congenital syphilis was broadened in 1989 and now includes all live or stillborn infants delivered to women with untreated or inadequately treated syphilis at delivery." (reference for quote:Sheila A. Lukehart. Chapter 153. "Syphilis" in Dennis L. Kasper, Eugene Braunwald, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Kurt J. Isselbacher, Eds.Harrison's Principles of Internal Medicine, 16th Edition)Before that time, cases were only counted if the infant was diagnosed with the infection. Now, if the mother has the infection and has not been adequately treated, infants are resumed to be infected as well.
Gonorrhea
When men and women are newly infected with gonorrhea, the symptoms depend on the route of entry. For both men and women the genital tract is usually infected. In men, there is usually a discharge from the penis. In women, the infection in the early stages is rarely has any signs or symptoms. Despite that, it is women who more commonly have the more serious problems from gonorrhea. That's because she is unlikely to seek treatment unless informed of the risk of disease by the man who infected her, and, without antibiotic treatment, the bacteria will often go on to infect the upper reproductive tract, causing inflammation and scarring of the fallopian tubes (salpingitis) and go on to cause infertility.
"The history of sexually transmitted diseases is thought to date back to earliest times, and many ancient texts describe conditions that may be those of syphilis and gonorrhea, which at one time were thought to be the same disease."(ref: Ligon BL. Albert Ludwig Sigesmund Neisser: discoverer of the cause of gonorrhea. Seminars in Pediatric Infectious Diseases. 16(4):336-41, 2005 Oct. UI: 16210113]] Ulcers on the genitals that appeared on men and women after sexual intercourse are described in Egyptian papyri. "A 12th century commentator, Rabbi Shlomo Yitzhati, wrote that the Hebrew word "Zav" ("issue") described a discharge the colour of "rice water". Celsus (25 BC--50 AD) described profusio seminis as the shedding of semen which occurs without sexual desire or erotic dreams, and in such a way that in time, the patient is consumed by wasting. [4] Galen (130-200 AD) originated the word gonorrhoea (Greek gonos, semen, and rhoia, to flow). He defined it as "an unwanted secretion of semen without erection."" (reference for quote:Oriel JD. The history of non-gonococcal urethritis. Genitourinary Medicine. 72(5):374-9, 1996 Oct. UI: 8976858)
After the epidemic of syphilis began in the 15th and 16th centuries, some physicians thought that it was the same illness as gonorrhea, but by the 18th century, it was accepted that there was a distinction in the two diseases. Certainly, we know that some patients are infected with both, and that must have added to the confusion over diagnosis.
The organism that causes Gonorrhea is also a bacteria, but unlike the spirochete that causes syphilis, this is a bacteria that is of a much more common shape and kind in terms of human infection, and that has remained much more sensitive to complete eradication by antibiotics throughout all stages of infection. None the less, although gonorrhea is generally a much more limited disease than syphilis, it can cause lesions in multiple organs and, in women, is associated with pelvic inflammatory disease.
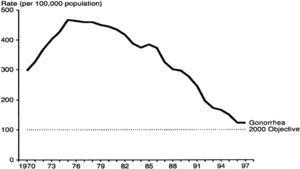
The infecting organism is the diplococcus bacteria Neisseria gonorrhoeae, which is negative on Gram stain."The introduction of treatment for gonorrhea also resulted in a decline in incidence during the 1950s, but, unlike syphilis, periodic oscillations did not ensue".
"There is no known protective immunity for uncomplicated gonococcal infection; a person can have repeated infections. The highly variable surface antigens help gonococci to evade antibodies and repeatedly infect humans."(ref Chapter 280- GONOCOCCAL INFECTIONS in H. David Humes, Herbert L. DuPont et al (Eds) :Kelley's textbook of internal medicine.—4th ed.ISBN 0781717876)
Chancroid
Chancroid is a venereal disease most common in Africa, and the developing world. Caused by the bacteria Hemophilius ducreyi, the hallmark of this disease is giant genital ulcers. Although some women are colonized by the bacteria without developing lesions, others do develop ulcers. It is men, however-particularly uncircumcised men, that bear the bulk of the lesions of this disease.Since women may be infected and harbor the bacteria without obvious disease, it is asymptomatic infected women who are primary carriers. About half of the men and women with ulcers also have enlarged lymph nodes in the groin (inguinal lymphadenopathy). The tissue in the center of these lymph glands often dies, becoming necrotic, and the mass in the groin then becomes soft and fluctuant. Rupture of these masses with spontaneous drainage may occur. Greatly enlarged lymph nodes with spontaneous rupture in this manner are sometimes called buboes, and are also a mark of plague.
Many people have called AIDS a modern plague, and chancroid is particlularly harmful in areas where HIV, the human immunodeficiency virus that causes AIDS, is prevalent . The patent with chancroid is at higher risk for HIV infection because the open ulcers offer a wide portal of entry. These open ulcers in men are one route of female-male HIV infection that helps account for the equal incidence of AIDS seen in men and women in Africa.
Venereal disease of viral origin
The venereal diseases listed here are caused by the transmission of viruses. Even so, the symptoms that they cause, in some cases, may be mistaken for venereal diseases spread by bacteria and for other illnesses, that are non-venereal in nature.
Herpes simplex

Genital herpes, syphilis, and chancroid are the most prevalent causes of genital ulcers. Genital herpes, unlike syphilis or chancroid, is caused by a virus and therefore, like all viruses, is not treatable with antibiotics. At this time, although there are anti-viral treatments for the Herpes simplex viruses that cause genital herpes;there is no cure. Once contracted, herpes is a lifelong disease characterized by recurrent outbreaks.
Human papillomavirus (HPV)
Human papilloma virus (HPV) is a viral wart that includes strains spread by sexual contact. Like some other venereal diseases, these strains can also be contracted by infants from their mothers. Certain types of the sexually transmitted virus have a high rate of malignant transformation of infected cells. The cells that the virus infects are epthelial cells, either skin cells or mucosa cells, and the transformation is to squamous cell carcinoma. The potential for a viral strain to cause malignant transformation is called " oncogenic potential". This oncogenic effect is most common in women with cervical infections, and is the single major cause of cervical cancer, but it also occurs in anal lesions in both men and women, causing anal squamous cell carcinoma, and squamous cell carcinoma of the lung, larynx and bronchi in children with congenital laryngeal papillomatosis.
"More than 100 HPV types are recognized, and individual types are associated with specific clinical manifestations. For example, HPV-1 causes plantar warts, HPV-6 causes anogenital warts, and HPV-16 infection can produce cervical dysplasia and invasive cervical cancer." (reference for quote:Richard C. Reichman. Chapter 169. Human Papillomavirus Infections in Dennis L. Kasper, Eugene Braunwald, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Kurt J. Isselbacher, Eds.Harrison's Principles of Internal Medicine, 16th Edition) "At least 30 HPV types infect the genital area, of which 15 are classified as high risk, that is, having oncogenic potential"(reference for quote:Barnabas RV, Laukkanen P, Koskela P, Kontula O, Lehtinen M, et al. Epidemiology of HPV 16 and Cervical Cancer in Finland and the Potential Impact of Vaccination: Mathematical Modelling AnalysesPLoS Medicine Vol. 3, No. 5, e138 doi:10.1371/journal.pmed.0030138).
Recent studies have suggested that condoms are not highly effective in preventing HPV infection.
Cervical cancer
Epidemiologic studies combined with mathematical modelling indicate that universal vaccination of young women is likely to markedly decrease the incidence of cervical cancer. Barnabas RV, Laukkanen P, Koskela P, Kontula O, Lehtinen M, et al. Epidemiology of HPV 16 and Cervical Cancer in Finland and the Potential Impact of Vaccination: Mathematical Modelling AnalysesPLoS Medicine Vol. 3, No. 5, e138 doi:10.1371/journal.pmed.0030138
HIV
Unlike the other venereal diseases discussed here, human immunodeficiency viruses does not affect the appearance of the genitals or other entry site into the body. Instead, there is a systemic infection that lodges in a certain type of white blood cell, the lymphocyte, of the new host.
Summary overview
Public health and infectious disease experts relate the incidence of venereal diseases to several factors. The first is the rate of spread, in venereal diseases that is related both to the number of infected people, how often susceptible people have sex with those who are infected, and how frequently each infected person has sex with new contacts. The second is how long the infected people remain both infected and sexually active, the longer that duration, the greater the spread. The third is how efficiently the disease is spread with each exposure to a susceptible person. Although male condoms can markedly decrease the efficiency of spread of these diseases, they do not prevent spread altogether. Some of the diseases, like chancroid or herpes, that cause open "wounds" on the genitals, increase the chances of catching other venereal diseases from an infected partner, notably HIV. HIV, by decreasing immune response, lowers the resistance to the HIV infected person to most infections, and notably to certain of the venereal diseases, like syphilis. For example, co-infection with HIV increases syphilis' severity, and, in particular, increases the likelihood that syphilis will affect the brain and central nervous system.