Vasopressin
| |
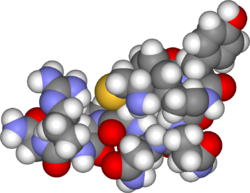
| Space-filling model of arginine vasopressin | |
arginine vasopressin (antidiuretic hormone)
| |
| Identifiers | |
| Symbol(s) | AVP VP, ADH |
| Entrez | 551 |
| OMIM | 192340 |
| RefSeq | NM_000490 |
| UniProt | P01185 |
| Other data | |
| Locus | Chr. 20 p13 |
Arginine vasopressin (AVP), also known as antidiuretic hormone (ADH) or argipressin, is a human hormone that is mainly released when the body is low on water; it causes the kidneys to conserve water by concentrating the urine and reducing urine volume. It also has various functions in the brain and blood vessels.
A very similar substance, lysine vasopressin (LVP) or lypressin, has the same function in pigs and is often used in human therapy.
These vasopressins are peptide hormones produced in the hypothalamus. Most of the processed peptide is stored in the posterior part of the pituitary gland to be released into the blood stream; some of it is also released directly into the brain.
Physiology
Control
AVP is secreted from the posterior pituitary gland in response to reductions in plasma volume and in response to increases in the plasma osmolality. Secretion in response to reduced plasma volume is activated by pressure receptors in the veins, atria, and carotids. Secretion in response to increases in plasma osmotic pressure is mediated by osmoreceptors in the hypothalamus. The neurons that make AVP, in the supraoptic nucleus and paraventricular nucleus, are themselves osmoreceptors, but they also receive synaptic input from other osmoreceptors located in regions adjacent to the anterior wall of the third ventricle. These regions include the organum vasculosum of the lamina terminalis and the subfornical organ.
Many factors influence the secretion of AVP; for instance, ethanol and caffeine reduce AVP secretion. The resulting decrease in water reabsorption by the kidneys leads to a higher urine output. Angiotensin II stimulates the secretion of AVP.[1]
The AVP that is measured in peripheral blood is almost all derived from secretion from the posterior pituitary gland (except in cases of AVP-secreting tumours). However there are two other sources of AVP with important local effects:
- AVP is secreted from parvocellular neurons of the paraventricular nucleus at the median eminence into the short portal vessels of the pituitary stalk. These vessels carry the peptide directly to the anterior pituitary gland, where it is an important releasing factor for ACTH, acting in conjunction with CRH.
- AVP is also released into the brain by several different populatons of neurons (see below).
Peripheral actions
AVP acts on three different receptors, termed AVPR1a, AVPR1b and V2. The receptors are differently expressed in different tissues, and exert different actions:
- AVPR1a - vasoconstriction, gluconeogenesis in the liver, platelet aggregation and release of factor VIII and von Willebrand factor.
- AVPR1b - corticotropin secretion from the pituitary gland.
- AVPR2 - control of free water reabsorption in the collecting ducts of the kidneys (especially the cortical and outer medullary collecting ducts). Activation of adenylate cyclase causes increase in cAMP which leads to the insertion of aquaporin-2 (AQP2) channels (water channels) into the apical membrane of the cells lining the collecting duct. This allows water to be reabsorbed down an osmotic gradient, and so the urine is more concentrated.
Actions within the brain
Vasopressin released within the brain has many actions:
- It has been implicated in memory formation, including delayed reflexes, image, short- and long-term memory, though the mechanism remains unknown, and these findings are controversial. However, the synthetic vasopressin analogue desmopressin has come to interest as a likely nootropic.
- AVP is released into the brain in a circadian rhythm by neurons of the suprachiasmatic nucleus of the hypothalamus.
- AVP released from centrally-projecting hypothalamic neurons is involved in aggression, blood pressure regulation and temperature regulation.
In recent years there has been particular interest in the role of AVP in social behavior. It is thought that AVP, released into the brain during sexual activity, initiates and sustains patterns of activity that support the pair-bond between the sexual partners; in particular, AVP seems to induce the male to become aggressive towards other males.
Evidence for this comes from experimental studies, in several species, which indicate that the precise distribution of AVP and AVP receptors in the brain is associated with species-typical patterns of social behavior. In particular, there are consistent differences between monogamous species and promiscuous species in the distribution of AVP receptors, and sometimes in the distribution of AVP-containing axons, even when closely-related species are compared. Moreover, studies involving either injecting AVP agonists into the brain, or blocking the actions of AVP, support the hypothesis that AVP is involved in aggression towards other males. There is also evidence that differences in the AVP receptor gene between individual members of a species might be predictive of differences in social behavior.
Structure and relation to oxytocin
The vasopressins are peptides consisting of nine amino acids (nonapeptides). (NB: the value in the table above of 164 amino acids is that obtained before the hormone is activated by cleavage). The amino acid sequence of AVP is Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly, with the cysteine residues form a sulfur bridge. Lysine vasopressin has a lysine in place of the arginine.
The structure of oxytocin is very similar to that of the vasopressins: it is also a nonapeptide with a sulfur bridge and its amino acid sequence differs at only two positions (see table below). These two neuropeptides are encoded by genes that arose through duplication approximately 400 million years ago. The two genes are located on the same chromosome separated by a relatively small distance of less than 15,000 bases in various species. The magnocellular neurons that make AVP are adjacent to magnocellular neurons that make oxytocin, and are similar in many respects. The similarity of the two peptides can cause some cross-reactions: oxytocin has a slight antidiuretic function, and high levels of AVP can cause uterine contractions.
Here is a table showing the superfamily of vasopressin and oxytocin neuropeptides:
Vertebrate Vasopressin Family Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2 Argipressin (AVP, ADH) Most mammals Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Lys-Gly-NH2 Lypressin (LVP) Pigs, hippos, warthogs, some marsupials Cys-Phe-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2 Phenypressin Some marsupials Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Arg-Gly-NH2 Vasotocin† Non-mammals Vertebrate Oxytocin Family Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Leu-Gly-NH2 Oxytocin (OXT) Most mammals, ratfish Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Ile-Gly-NH2 Mesotocin Most marsupials, all birds, reptiles, amphibians, lungfishes Cys-Tyr-Ile-Ser-Asn-Cys-Pro-Ile-Gly-NH2 Isotocin Bony fishes Cys-Tyr-Ile-Asn/Gln-Asn-Cys-Pro-Leu/Val-Gly-NH2 Various tocins Sharks Invertebrate VP/OT Superfamily Cys-Leu-Ile-Thr-Asn-Cys-Pro-Arg-Gly-NH2 Diuretic Hormone Locust Cys-Phe-Val-Arg-Asn-Cys-Pro-Thr-Gly-NH2 Annetocin Earthworm Cys-Phe-Ile-Arg-Asn-Cys-Pro-Lys-Gly-NH2 Lys-Connopressin Geography & imperial cone snail, pond snail, sea hare, leech Cys-Ile-Ile-Arg-Asn-Cys-Pro-Arg-Gly-NH2 Arg-Connopressin Striped cone snail Cys-Tyr-Phe-Arg-Asn-Cys-Pro-Ile-Gly-NH2 Cephalotocin Octopus Cys-Phe-Trp-Thr-Ser-Cys-Pro-Ile-Gly-NH2 Octopressin Octopus †Vasotocin is the evolutionary progenitor of all the vertebrate neurohypophysial hormones. Only vasotocin found in hagfish & lampreys (Agnatha appeared 500 million years ago)
Role in disease
Decreased AVP release or decreased renal sensitivity to AVP leads to diabetes insipidus, a condition featuring hypernatremia (increased blood sodium content), polyuria (excess urine production), and polydipsia (thirst).
High levels of AVP secretion (syndrome of inappropriate antidiuretic hormone, SIADH) and resultant hyponatremia (low blood sodium levels) occurs in brain diseases and conditions of the lungs. In the perioperative period, the effects of surgical stress and some commonly used medications (e.g., opiates, syntocinon, anti-emetics) lead to a similar state of excess AVP secretion. This may cause mild hyponatraemia for several days.
Pharmacology
Vasopressin analogues
AVP agonists are used therapeutically in various conditions, and its long-acting synthetic analogue desmopressin is used in conditions featuring low AVP secretion, as well as for control of bleeding (in some forms of von Willebrand disease) and in extreme cases of bedwetting by children. Terlipressin and related analogues are used as vasocontrictors in certain conditions. Use of AVP analogues for esophageal varices commenced in 1970.[2]
AVP infusion has been used as a second line of management in septic shock patients not responding to high dose of inotropes (e.g., dopamine or epinephrine). It had been shown to be more effective than epinephrine in asystolic cardiac arrest. [3] While not all studies are in agreement, a 2006 study of out-of hospital cardiac arrests has added to the evidence for the superiority of AVP in this situation. [4]
Vasopressin receptor inhibition
Demeclocycline, a tetracycline antibiotic, is sometimes used to block the action of AVP in the kidney in hyponatremia due to inappropriately high secretion of AVP (SIADH, see above), when fluid restriction has failed. A new class of medication (conivaptan, tolvaptan, relcovaptan, lixivaptan) acts by inhibiting the action of AVP on its receptors (V1 and V2), with tolvaptan acting on V1a and V2 and the remainder mainly on V1a receptors. The same class of drugs is also being studied in congestive heart failure.
References
- ↑ Vander, A.J., Renal Physiology, McGraw-Hill, 1991.
- ↑ Baum S, Nusbaum M, Tumen HJ. The control of gastrointestinal hemorrhage by selective mesenteric infusion of pitressin. Gastroenterology 1970;58:926.
- ↑ Wenzel V, Krismer AC, Arntz HR, Sitter H, Stadlbauer KH, Lindner KH; European Resuscitation Council Vasopressor during Cardiopulmonary Resuscitation Study Group. A comparison of AVP and epinephrine for out-of-hospital cardiopulmonary resuscitation. N Engl J Med 2004;350:105-13. PMID 14711909.
- ↑ Grmec S, Mally S. Vasopressin improves outcome in out-of-hospital cardiopulmonary resuscitation of ventricular fibrillation and pulseless ventricular tachycardia: a observational cohort study. Crit Care. 2006 Feb;10(1):R13. PMID 16420660.
- Brenner & Rector's The Kidney, 7th ed., Saunders, 2004. Full Text with MDConsult subscription
- Caldwell, H.K. and Young, W.S., III. Oxytocin and Vasopressin: Genetics and Behavioral Implications in Lim, R. (ed.) Handbook of Neurochemistry and Molecular Neurobiology, 3rd edition, Springer, New York, pp. 573-607, 2006. 320kb PDF