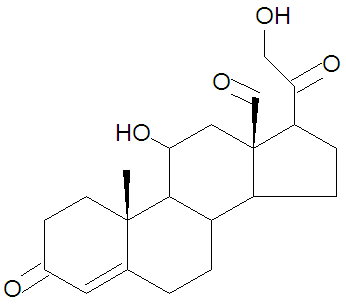
Aldosterone
Aldosterone, also called (11ß)-11,21-Dihydroxy-3,20-dioxo-pregn-4-en-18-al, is a steroid hormone. It is the major mineralcorticoid hormone and has a critical role in regulating the concentrations of sodium and potassium - in extracellular fluids, thereby influencing blood pressure and hydration. A deficiency in mineralocorticoids can lead to life-threatening abnormalities of electrolyte and fluid balance.
Aldosterone acts mainly at the distal tubule of the kidney. There, it promotes the resorption of sodium, meaning that less sodium is lost from the body in urine. It also increases resorption of water, producing an expansion in the volume of the extracellular fluid; this is an osmotic effect that is directly related to the increased resorption of sodium. Finally, it increases the rate at which potassium is excreted.
Aldosterone acts via mineralocorticoid receptors to stimulates transcription of the gene encoding the sodium-potassium ATPase. This leads to an increase in the number of "sodium pumps" in the basolateral membranes of tubular epithelial cells. Aldosterone also increases the expression of a sodium channel which facilitates uptake of sodium from the tubular lumen. Aldosterone also has similar effects on sweat glands, salivary glands and the colon. Together, the result is that aldosterone acts to conserve body sodium and water.
The mineralocorticoid receptor binds aldosterone and cortisol with equal affinity - and the same DNA sequence is a response element for the activated forms of both mineralocorticoid and glucocorticoid receptors. As the plasma concentrations of glucocorticoids (cortisol in humans) are very much higher than those of aldosterone, the target cells for aldosterone have to be "protected" from the effects of cortisol. These cells express the enzyme 11-beta-hydroxysteroid dehydrogenase which converts cortisol to a relatively inactive metabolite, cortisone, allowing aldosterone to bind to mineralocorticoid receptors without interference.
Aldosterone secretion is stimulated when the concentration of potassium ions in extracellular fluid is raised, and inhibited when the concentration of sodium is raised. When blood volume falls, the renin-angiotensin system is activated as a result of decreased renal blood flow and this results in release of angiotensin II, which stimulates aldosterone secretion. Adrenocorticotropic hormone can also produce a transient increase in aldosterone secretion.
Aldosterone is synthesized from corticosterone by oxidation of the C-18 methyl group to form an aldehyde.
Primary aldosteronism
Primary aldosteronism underlies about 10% of cases of resistant hypertension.[1]
Clinical practice guidelines are available for managing primary aldosteronism.[2] A aldosterone renin ratio (ARR) over 20 with an elevated aldosterone level suggests primary hyperaldosteronism.[2]
References
- ↑ Douma S, Petidis K, Doumas M, et al (June 2008). "Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study". Lancet 371 (9628): 1921–6. DOI:10.1016/S0140-6736(08)60834-X. PMID 18539224. Research Blogging.
- ↑ Jump up to: 2.0 2.1 Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M et al. (2008). "Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline.". J Clin Endocrinol Metab 93 (9): 3266-81. DOI:10.1210/jc.2008-0104. PMID 18552288. Research Blogging. Free fulltext